Soap Note Example Uti . ***instructed to force fluids/take medicine until it is gone/if the symptoms. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti.
from www.studocu.com
Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms.
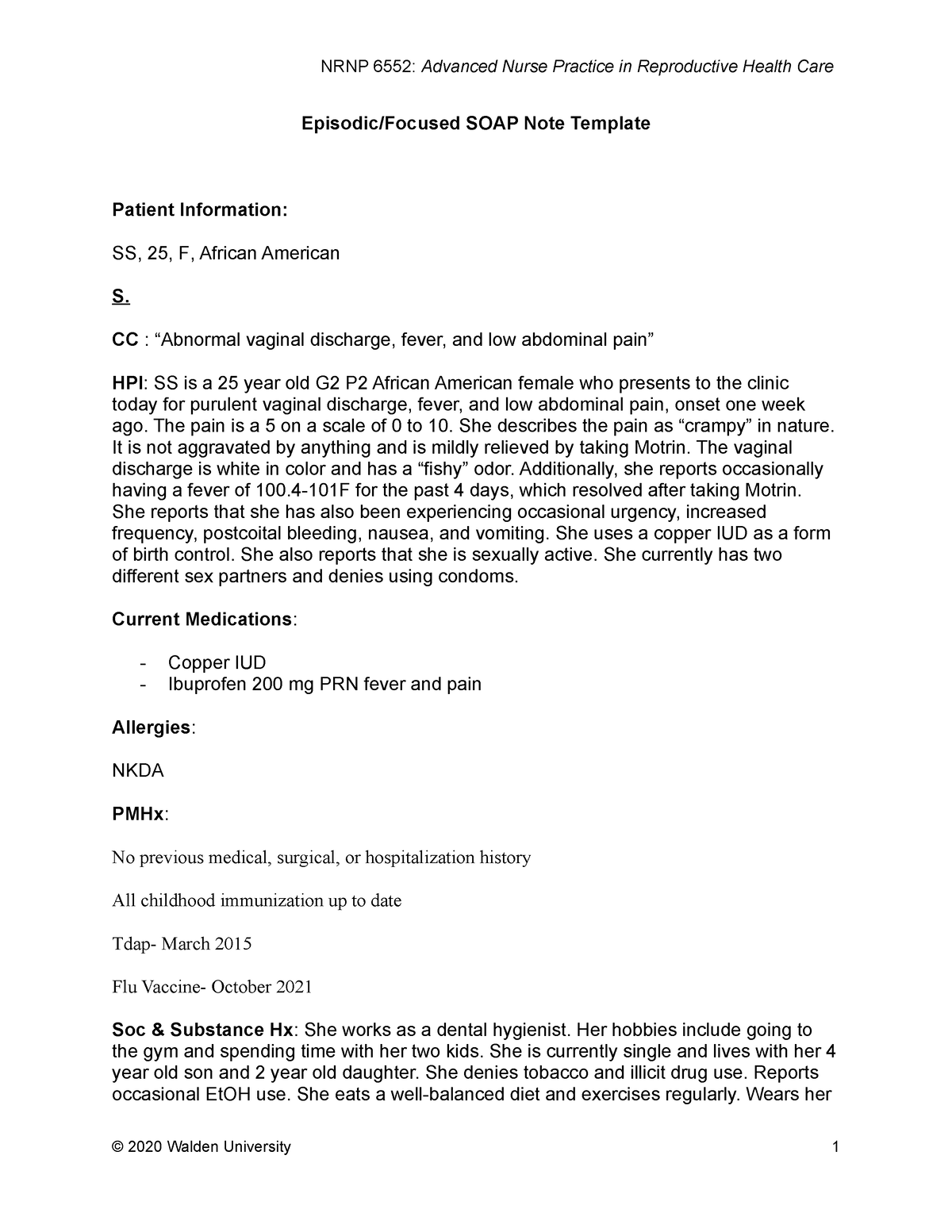
Wk5 soap soap note about STIs. Includes differential diagnosis
Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms.
From www.studypool.com
SOLUTION Soap note urinary tract infection Studypool Soap Note Example Uti ***instructed to force fluids/take medicine until it is gone/if the symptoms. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. Soap Note Example Uti.
From one.wkkf.org
Slp Soap Note Template Soap Note Example Uti ***instructed to force fluids/take medicine until it is gone/if the symptoms. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. Soap Note Example Uti.
From www.pinterest.com
Soap Note Template Nurse Practitioner Lovely What is A soap Note Soap Soap Note Example Uti The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. Soap Note Example Uti.
From studylib.net
Patient SOAP Note Charting Procedures Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. Soap Note Example Uti.
From www.youtube.com
How to Write SOAP Notes YouTube Soap Note Example Uti ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.
From www.studocu.com
Episodic Focused SOAP Note Template Episodic/Focused SOAP Note Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap Note Example Uti.
From www.etsy.com
Peds SOAP Note for UTI Etsy Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.
From www.etsy.com
SOAP Note Guide and Real Example for Nurse Practitioners Etsy Soap Note Example Uti Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. ***instructed to force fluids/take medicine until it is gone/if the symptoms. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.
From www.scribd.com
Soap Notes Guidelines Diet (Nutrition) Nutrition Soap Note Example Uti ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.
From www.carepatron.com
SOAP Notes for Therapy Template & Example Free PDF Download Soap Note Example Uti Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap Note Example Uti.
From www.carepatron.com
SOAP Notes Template & Example Free PDF Download Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap / chart / progress notes. Soap Note Example Uti.
From therapistsmarket.com
Simple SOAP Note Template by a Licensed Therapist Soap Note Example Uti [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. Soap / chart / progress notes. ***instructed to force fluids/take medicine until it is gone/if the symptoms. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab Soap Note Example Uti ***instructed to force fluids/take medicine until it is gone/if the symptoms. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. Soap Note Example Uti.
From www.typecalendar.com
Free Printable SOAP Note Templates [PDF, Word] Soap Note Example Uti The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. Soap / chart / progress notes. Soap Note Example Uti.
From www.scribd.com
Soap Note 4 (CPII) Urinary Tract Infection Public Health Soap Note Example Uti Soap / chart / progress notes. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. Soap Note Example Uti.
From www.pinterest.com.au
3+ SOAP Note Example Free Download Soap note, Nursing notes examples Soap Note Example Uti The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap Note Example Uti.
From www.scribd.com
Obgyn Soap Note Example Vagina Mammal Female Reproductive System Soap Note Example Uti Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. ***instructed to force fluids/take medicine until it is gone/if the symptoms. Soap Note Example Uti.
From www.typecalendar.com
Free Printable SOAP Note Templates [PDF, Word] Soap Note Example Uti Soap / chart / progress notes. [text size=”3″] year old f pt presents to the clinic today with symptoms of a uti. ***instructed to force fluids/take medicine until it is gone/if the symptoms. The subjective, objective, assessment and plan (soap) note is an acronym representing a widely used method of documentation for healthcare providers. Soap Note Example Uti.